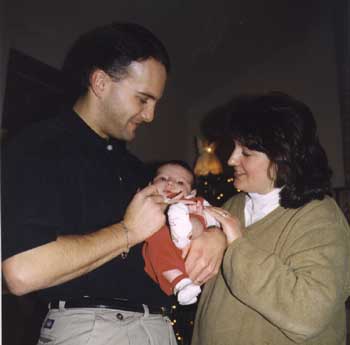
anguished parents through transplant wait "We're not leaving anyone behind" Mark and Stephanie Laubacher of Ogden are having a Christmas they'll always remember. It's 'baby's first Christmas,' but it's also the first time they have been home with their new little Megan Cecelia, an angelic girl whose fight for life took the adults around her on a difficult and tearful journey. Their story begins September 26 at Highland Hospital Maternity where Stephanie, an accountant by profession, and Mark, manager of Communication and Technology Services at Monroe-Orleans BOCES No. 2, joyfully welcomed Megan into the world. "It was a perfect pregnancy," Stephanie said. But within weeks their lives would revolve around Neo-Natal Intensive Care at Strong Memorial Hospital … an infant gasping for breath as her heart beat out of control … and then life-threatening complications which led to a transfer to the Children's Hospital in Pittsburgh for a possible heart transplant. "After many lab tests, we found out that Megan was a transplant candidate," Mark said. "What began as a heart murmur shortly after birth, was found to be an enlarged heart, then a block in the aorta." The Laubachers flew Megan to Children's Hospital of Pittsburgh for a heart transplant evaluation. They were unprepared for the scope of what they saw: floor after floor of sick and dying infants and children, parents living on the edge every day. Some days up and others down. And all families experiencing one form of grief and tears or another. Children's Hospital, one of the nation's preeminent transplant facilities for children, helped the Laubachers stay at the Ronald McDonald house in Pittsburgh where they became close with many parents awaiting transplant for their children. World-class pediatric cardiologists evaluated Megan and recommended a heart transplant for the "very, very sick" child. "She had a coarctation of the aorta, a blockage," Stephanie said, painfully remembering each diagnostic test as if it were yesterday. "It is a narrowing in her aorta which wasn't allowing her heart to get enough oxygen, causing her heart to work too hard." Through MRIs and X-Rays, EKGs, and numerous echocardiograms, the infant was found to be a good transplant candidate … if she could live that long. "She was very lethargic, wouldn't eat," Stephanie said. "She had trouble breathing. She had to be on a respirator, a feeding tube, IVs for medication." But the baby started to show signs of a stronger heart and in October, at three-and-a-half weeks, she underwent a special aortic surgery that would remove the blockage and stretch her artery across that gap. "A transplant of any kind is a one-way street," Mark said. "You have to be on anti-rejection drugs for the rest of your life … There's a 90 percent success rate for the transplant, but your biggest risk is waiting for the organ to become available." The Laubachers learned that infants with Megan's condition constitute less than one percent of all newborns. As they waited and watched their baby struggle for life, unable to hold her and help her deal with the pain, a little miracle was happening in their child. Her cardiac output kept increasing. By three weeks after the surgery, there was a "significant" improvement. Following transfusions, up to 20 different medications at any one point, and potent painkillers, too powerful for an infant, Megan continued to gain strength. In early December she was flown home and today she continues to improve. "People around us felt helpless through all of this," Mark said. "They prayed … prayer lists and prayer chains … and I'm convinced that their prayers worked." Both parents were strengthened by their daughter's happy personality which shown through her sparkling eyes. "She is our strength," Mark said. "At this point, doctors feel she will come off the transplant list and she will recover." "Babies are so resilient," Stephanie said, "because of their tissues' ability to regenerate cells." "But we left a lot of kids behind," Mark added. "We made a promise that we would not forget them and we would work for promotion of organ donation. Parents can wait for as long as a year for a transplant. We saw one child pass away. The greatest risk is the wait - surviving long enough to receive a transplant. We found out that 90 percent of people who could be organ donors are not." The Laubachers are correct. Seven thousand New Yorkers are awaiting transplants. According to the N.Y.S. Organ and Tissue Donor Registry (www.health.state.ny.us), there is a "severe shortage of organs and tissues for transplantation." As of November 2001, according to the U.S. Department of Health and Human Services Organ Donation web site (www.organdonor.gov), 79,000 people nationwide are awaiting tissue transplants; 50,000 need kidney; 19,000 need liver; 4,000 need heart; 4,000 need lungs; 2,000 need kidney/pancreas; 2,000 need pancreas; 300 need pancreatic islet; 200 need heart/lung; 200 need intestine. Some of these numbers represent multiple organ needs. Last year, 22,953 transplants were done, according to the Department of Health and Human Services, but for many, the wait is agonizingly long and often results in death. What can you do about this? New Yorkers have the option of checking off on the back of their driver's license the consent to donate organs, but in addition to this consent, the family of the deceased is required to give consent also. "Families need to sit down and talk to each other about this before a crisis occurs," Mark Laubacher said. Anyone can become a donor according to the N.Y.S. Donor Registry and potential donors can register their consent on-line. What registry does is link the donor's name with the local organ procurement agency. In our area that is the Finger Lakes Donor Recovery Network, 30 Corporate Woods, Suite 220, Rochester, NY 14623. They may be reached at 716-272-4930. According to the Donor Registry, one person who donates organs (heart, lung, kidneys, pancreas, intestines) can save up to eight lives, while a tissue donor (corneas, bone, skin, heart valves, tendons, veins, etc.) can improve the lives of 12 or more people. Hilton High School Director of Human Resources, Eric Wright, who suffers from cystic fibrosis and CF-related diabetes, has looked into organ transplant for himself. At age 30, his lung capacity is severely diminished due to the disease. Eric would need a double-lung transplant, but his lung output is still strong enough to keep him off the transplant list. "I'm trying to stay healthy," he said. "I have joined a gym and have a trainer who works with me to use oxygen more efficiently. I already have established a transplant fund and if I can help it, I'll do everything I can to keep my lung capacity up." The Laubachers continue to carry the message of organ donation to everyone who will listen. "What better gift can you give than the gift of life?" Mark said. "The most precious gift is to see your loved one go on living in someone else. Families are presented with the question of organ donation at the most difficult time. The decision needs to be made before you are faced with a tragedy." Megan's heart continues to grow stronger. "She's not out of the woods yet," Mark said, "but not everybody has a happy ending like we do. Many are still waiting." The Laubachers urge everyone to consider a special Christmas gift this year. Contact the N.Y.S. Organ and Tissue Registry or our local agency at 1-800-810-5494. |