Nursing homes see 96 percent decline in COVID cases since vaccine rollout
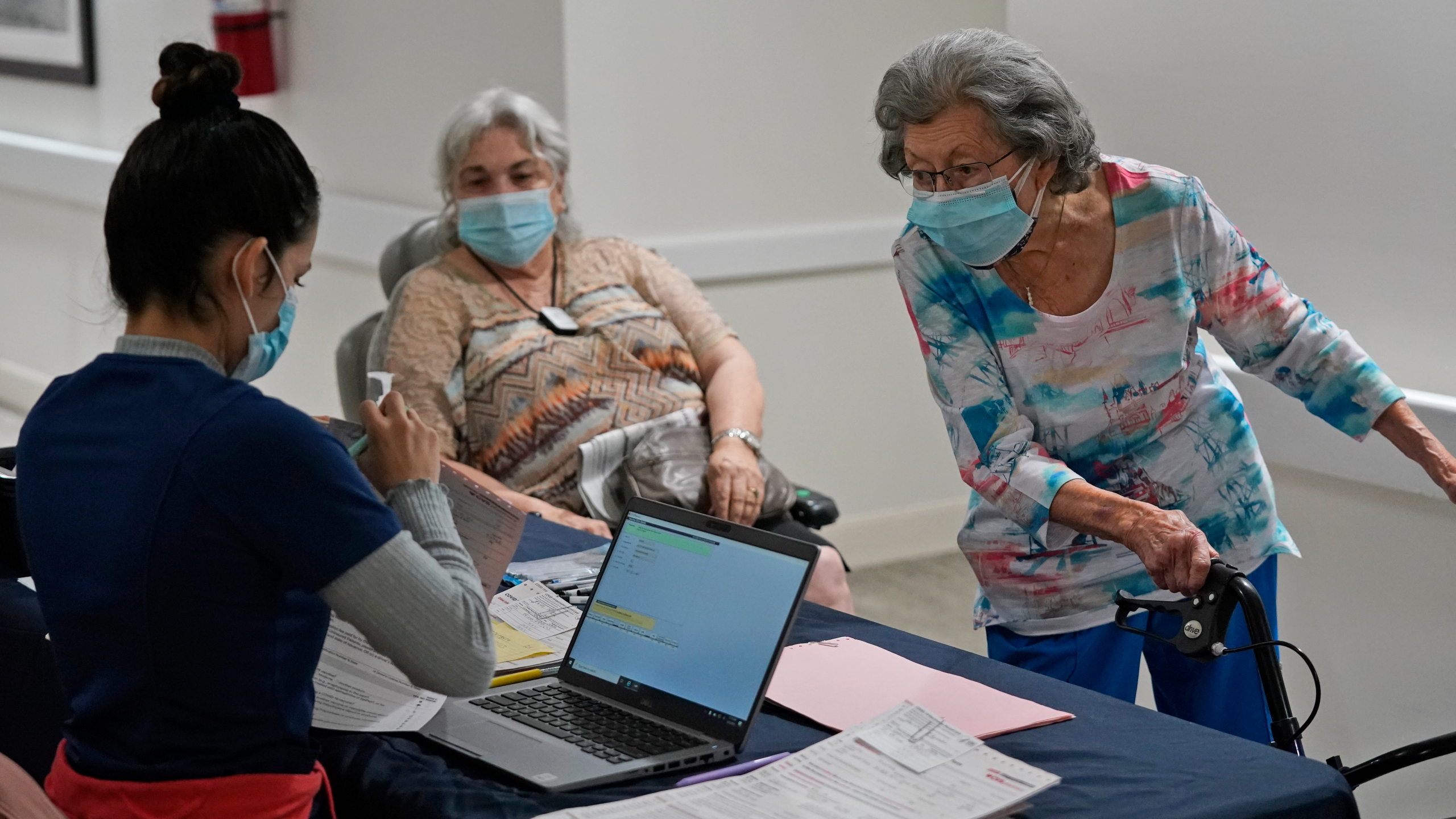
The American Health Care Association and National Center for Assisted Living (AHCA/NCAL), representing more than 14,000 nursing homes and long term care facilities across the country that provide care to approximately five million people each year, recently released a report showing nursing homes in the U.S. continue to see a rapid decline in new COVID-19 cases thanks to initial vaccine allocations prioritized for nursing homes. They are also calling on Congress to consider the industry’s Care For Our Seniors Act to address systemic issues facing the nursing home sector and prevent another COVID-type crisis.
Recent CMS data shows that nursing homes have seen a 96 percent decline in new COVID cases among residents since the peak during the week of December 20 of last year when there were more than 30,000 new resident cases. Along with the lowest number of new COVID cases, AHCA/NCAL’s new report shows COVID related deaths in nursing homes declined by 91 percent since December 20, 2020.
“We are not out of the woods yet, but these numbers are incredibly encouraging and a major morale booster for frontline caregivers who have been working tirelessly for more than a year to protect our residents,” said Mark Parkinson, president and CEO of AHCA/NCAL. “This trend shows that when long term care is prioritized, as with the national vaccine rollout, we can protect our vulnerable elderly population. Now we need Congress to prioritize our nursing homes for the long-term by considering the initiatives in the Care For Our Seniors Act to improve the quality of care for our residents.”
AHCA and LeadingAge, recently released the reform agenda, the Care For Our Seniors Act, to address long-standing challenges affecting the quality of care provided in America’s nursing homes. The organizations say the COVID-19 pandemic has exposed and exacerbated systemic issues impacting the nursing home sector, such as workforce shortages, aging physical plants, and underfunded government reimbursements for care.
The Care For Our Seniors Act focuses on four key areas for improvement, which include enhancing the quality of care with enhanced standards for infection preventionists, requiring that each nursing home have a registered nurse on-staff 24 hours per day, and requiring a minimum 30-day supply of personal protective equipment in all nursing homes. The initiative also calls for a multi-phase, tiered approach to attract, retain, and develop more long term care professionals leveraging federal, state, and academic institutions.
While recommending several new ways to improve oversight and processes to support better care and protect residents, the Care For Our Seniors Act also aims to modernize nursing homes by looking at how the industry could shift to more private rooms, promoting resident privacy and supporting infection control best practices.
AHCA and LeadingAge say reform will be costly, but is long overdue. The nursing home sector has been facing a financial crisis for years even before COVID due to low Medicaid reimbursements, the primary coverage for nursing home residents. The Care For Our Seniors Act calls for an increase in federal Medicaid funds provided to states and bringing the Medicaid rate up to equal the cost of care. Currently, Medicaid only covers 70 to 80 percent of the costs to care for a nursing home resident.
“With a growing elderly population soon needing our services, the moment is now. We must pay tribute to all those who lost their lives to this vicious virus and resolve to bring forth a brighter future,” concluded Mark Parkinson, president and CEO of AHCA/NCAL. “We have already seen what progress can be made when policymakers come together to make long term care residents a priority and through these reforms, we can significantly improve the quality of care for our current residents and generations to come.”
To learn more about the Care For Our Seniors Act, visit www.ahcancal.org/
solutions.
Provided information





